
by Lucy Goodman | 11 Aug, 2022 | Eye care services, Resources
In 2020, the Government of Aotearoa New Zealand proposed free annual “eye health checks” for New Zealand’s ~700,000 SuperGold card holders aged ≥65 years. To assess the evidence for this policy, we conducted a systematic scoping review of primary eye care services in Aotearoa New Zealand and ten similar high-income countries. We found that most of the countries included in the review provided subsidised eye examinations for older people. New Zealand was the only country that did not provide any eye care services for older people.
Read the published research paper and a policy brief describing the implications of this research.
Citation: Goodman L, Hamm L, Tousignant B, et al. Primary eye health services for older adults as a component of universal health coverage: a scoping review of evidence from high income countries. Lancet Reg Health West Pac. 2023;35:100560. doi: 10.1016/j.lanwpc.2022.100560
Funding: Blind Low Vision New Zealand.

by Lucy Goodman | 2 Aug, 2022 | Eye care services, Resources
Key messages:
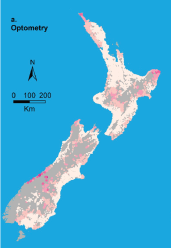
Travel distance is unlikely to be a barrier to accessing eye health services for most New Zealanders. However, there are communities in the most deprived areas that also have long distances to travel to eye clinics. These communities are often in areas with relatively more Māori. Making eye health services more accessible for these communities should be prioritised if we are to improve eye health in New Zealand equitably.
Read the published research paper and download a plain language summary of the findings.
Why did we do this research?
Some New Zealanders face many barriers to good eye health. One of these barriers could be the distance they must travel to reach services. To make eye health services more accessible, we need to understand which communities have furthest to travel, especially when those communities may already be under resourced.
In 2022, Community Eye Health researchers published their research reporting how far New Zealanders need to travel to reach their closest eye care provider. The research showed that people living in the most deprived areas of New Zealand sometimes have the longest distances to travel to eye clinics. To achieve equity in eye care, we need to make these services more accessible.
What was the aim of this research?
The aim of this research was to find out how far people need to travel to eye clinics (optometrists and ophthalmologists) across Aotearoa New Zealand. The researchers also identified communities in the most deprived areas that were more than 50 kilometres from eye clinics, because these communities might benefit from closer services.
What did we do?
To understand how far people travel for eye health services, our researchers used data held by Stats NZ Tatauranga Aotearoa to count and locate all New Zealanders. They then used the addresses of all optometry and ophthalmology clinics in Aotearoa to calculate the travel distance—along our road network—between each clinic and the population. They also calculated the proportion of New Zealanders living more than 50 kilometres from clinics, and looked at distances for people living in different districts and levels of area deprivation.
What are the main results?
The researchers found 344 optometry, 46 public ophthalmology and 90 private ophthalmology clinics. Three-quarters of New Zealanders lived within 10 km of an optometry clinic and half lived within 10 km of an ophthalmology clinic. Nationally, approximately 1 in 35 people lived further than 50km from an optometry clinic compared to 1 in 14 and 1 in 10 living further than 50km from public and private ophthalmology. The researchers identified communities with high area-level deprivation that were more than 50km from eye health services. These communities were predominantly in Tairāwhiti and Northland, but there were also some in Whanganui, Hawke’s Bay, Bay of Plenty and Waikato.
Citation: Ramke J, Zhao J, Wilson O, et al. Geographic access to eye health services in Aotearoa New Zealand: which communities are being left behind? Clin Exp Optom. 2023;106:158–64. doi: 10.1080/08164622.2022.2102410
Funding: Blind Low Vision New Zealand.

by Lucy Goodman | 27 Jul, 2022 | Pacific Islands, Resources
 In 2022, researchers from the Community Eye Health team (Pushkar Silwal, Renata Watene, Jacqueline Ramke) were commissioned to prepare a detailed report that summarises the state of eye care services in Aotearoa New Zealand. The report highlights that while New Zealand has a solid foundation for good quality eye care services, there is room for improvement in the way we plan and deliver eye care services to ensure all New Zealanders can access the services they need. Eye Care in Aotearoa New Zealand (2022) uses the World Health Organization’s Eye Care Situation Analysis Tool (ECSAT) to summarise the performance of our eye care services. The tool consists of 31 items (grouped into six ‘building blocks’) that each assess a different component of New Zealand’s eye care services.
In 2022, researchers from the Community Eye Health team (Pushkar Silwal, Renata Watene, Jacqueline Ramke) were commissioned to prepare a detailed report that summarises the state of eye care services in Aotearoa New Zealand. The report highlights that while New Zealand has a solid foundation for good quality eye care services, there is room for improvement in the way we plan and deliver eye care services to ensure all New Zealanders can access the services they need. Eye Care in Aotearoa New Zealand (2022) uses the World Health Organization’s Eye Care Situation Analysis Tool (ECSAT) to summarise the performance of our eye care services. The tool consists of 31 items (grouped into six ‘building blocks’) that each assess a different component of New Zealand’s eye care services.
Read the published report and download the plain language summary of the findings.
Why did we undertake an ECSAT?
Globally, more than a billion people live with vision impairment and the negative effects this can have on their lives. To reduce this problem, in its inaugural World report on vision, the World Health Organization called for eye health to be part of efforts to achieve universal health coverage (UHC) through implementing Integrated People-centred Eye Care across the spectrum of promotive, preventative, curative and rehabilitative services. In 2020, this call was adopted by 194 countries at the 73rd World Health Assembly (including Aotearoa). To improve our eye care services, we must first understand the strengths and weaknesses of current services. This understanding is enabled by ECSAT, which is the first of four tools in the Guide for Action developed by WHO to support countries to strengthen integration of eye care into the health system.
The ECSAT report was commissioned by Eye Health Aotearoa to support New Zealand’s policy makers to develop integrated people-centred eye care, and ensure that all New Zealanders can access quality care.
How did we prepare the report?
To prepare the report, we established a Technical Working Group that included members with experience in optometry, ophthalmology, primary care/general practice, rehabilitation and Māori health. We used information gathered from published documents, which we augmented by interviewing with people with detailed knowledge of eye care services. The report can be downloaded from the Open Science Framework.
The report was launched by Eye Health Aotearoa at Parliament on 27 July 2023.
What are the major findings of the report?
The report identified that components of our eye care services in Aotearoa that are generally “strong” or only “need minor strengthening”, include:
- Service delivery: The quality of eye care services.
- Workforce & infrastructure: Ensuring that workers are trained and available to provide eye care services.
In contrast, the components of our eye care services that had aspects that “need major strengthening” include:
- Leadership & governance: Planning, integrating and coordinating services, with appropriate policies in place.
- Financing: How services are funded, including reducing out-of-pocket costs for population groups who are less able to afford services.
- Access to services: Availability of the range of services throughout the country, as well as whether all population groups can access them.
- Information: How service performance is monitored, and whether evidence is used to inform how services operate.
The report provides a detailed list of 81 recommended actions that may help strengthen eye care services in New Zealand.
Citation: Silwal P, Watene R, Cowan C, Cunningham W, Harwood M, Korau J, Sue W, Wilson G, Ramke J. Eye care in Aotearoa New Zealand 2022: Eye care situation analysis tool (ECSAT). Auckland: University of Auckland, 2022. Available at: https://osf.io/r75zs/
Funding: The report was prepared for Eye Health Aotearoa, with funding from Blind Low Vision New Zealand.

by Lucy Goodman | 1 Jun, 2021 | Children, Resources
 Key messages:
Key messages:
The B4 School Check (B4SC) vision screening service is successfully delivered to most New Zealand preschool children. However, for some groups of children, the B4SC is less accessible and more likely to deliver an incomplete test measurement. This includes Māori and Pacific children, and those living in areas of higher deprivation or in particular regions of New Zealand.
Read the published paper and download a plain language summary of the findings.
About preschool vision screening
Preschool vision screening helps to identify children with eye problems. Early treatment can then prevent permanent vision loss and difficulties at school. In Aotearoa New Zealand, all children 4 years of age are offered a free vision screening test as part of the national B4SC screening programme, and children identified for further testing are referred to eye clinics for treatment. In principle, all children in New Zealand can participate in the B4SC. However, the B4SC is inaccessible for some children, for various reasons such as difficulties in scheduling an appointment. Sometimes the vision screening test is unable to be completed (for example, due to language barriers).
Why did we do this research?
We conducted this research to understand whether there are any inequities in the B4SC vision screening programme between children from different ethnicities, or living in areas with different levels of deprivation or in particular regions of New Zealand.
What did we do?
Using information from the Statistics New Zealand database, we counted the number of children in New Zealand aged 4 years between 1st July 2011 and 30th June 2015. For each child, we recorded their ethnicity, and the level of deprivation of the area they lived and the health district where they live. We calculated how many of these children accessed vision screening (the screening “coverage”), and how often the screening test was performed successfully (the screening “testability).
What did we find?
Screening coverage: Nearly 90% of children could access the B4SC. The B4SC was less accessible to children of Māori, Pacific, Asian, or other minority ethnicities, or living in more deprived areas. This service was also less accessible for children in the Capital and Coast health districts than those in other regions.
Screening testability: The test was successfully completed for almost all the children who participated (97.7%). Completed testing was lowest for children of Māori or Pacific ethnicity, or living in more deprived areas. Children in the Whanganui health district were more likely to have an unsuccessful screening test compared to other regions.
What’s next?
We need improve the way the B4SC vision screening programme is delivered so that it is equally accessible to all groups of children. In particular, this should involve consultation with Māori. Future research should examine why there are regional differences in screening rates across New Zealand.
Citation: Findlay R, Hamm L, Anstice N, et al. Vision screening in New Zealand pre-school children: Is it equitable? J Paediatr Child Health. 2021;57:1594–9. doi: 10.1111/jpc.15548.
Funding: A Better Start – National Science Challenge





 In 2022, researchers from the Community Eye Health team (Pushkar Silwal, Renata Watene, Jacqueline Ramke) were commissioned to prepare a detailed report that summarises the state of eye care services in Aotearoa New Zealand. The report highlights that while New Zealand has a solid foundation for good quality eye care services, there is room for improvement in the way we plan and deliver eye care services to ensure all New Zealanders can access the services they need.
In 2022, researchers from the Community Eye Health team (Pushkar Silwal, Renata Watene, Jacqueline Ramke) were commissioned to prepare a detailed report that summarises the state of eye care services in Aotearoa New Zealand. The report highlights that while New Zealand has a solid foundation for good quality eye care services, there is room for improvement in the way we plan and deliver eye care services to ensure all New Zealanders can access the services they need. 
 Key messages:
Key messages: