by Lucy Goodman | 26 Mar, 2024 | Eye care services, Resources
 Key messages
Key messages
New Zealand has very little evidence describing vision impairment or access to eye care services. Reassuringly, recent studies often compare their findings between Māori and Pacific People and other ethnic groups. The evidence we do have consistently reports that eye care services are less accessible to Māori and Pacific People compared to other ethnic groups.
Read the published paper and download the plain language summary of the findings.
Inequities in eye health
Health inequities are common in Aotearoa New Zealand. In particular, Māori experience poorer access to services and subsequently poorer health compared to other population groups in New Zealand. However, we don’t know if this is the case for eye health services, and eye health has received little attention by policy makers. To improve eye health, policy makers need to know the number of people and the population groups who are most in need of eye health services. While further research may be needed to answer these questions, some of the information could be identified from existing evidence.
Why did we do this research?
We wanted to identify and summarise all the existing evidence of inequities in eye health between different population groups—particularly between Māori and other ethnic groups. This will help us identify what types of research is still needed.
What did we do?
We looked for all published studies about eye health in New Zealand. Studies were eligible if they reported the number of people with impaired vision, or access to an eye care service (such as the number of people attending a vision screening service). We did this in a systematic way, by searching databases for published evidence and carefully screening the results using pre-defined criteria.
What did we find?
New Zealand has very little published evidence describing the prevalence of vision impairment or access to eye health services. We found 47 relevant studies published since 1960. Almost all this evidence comes from data collected from health facilities (e.g. hospitals), which means the information is not relevant to everyone in the population. Many studies were about diabetic retinopathy (an eye condition resulting from diabetes), or cataract. Since the year 2000, studies have consistently compared their findings between Māori or Pacific People and one or more other ethnic groups. These studies reported that Māori and Pacific People experienced worse access to services compared to other groups.
What’s next?
Future eye health services need to address barriers and enablers to eye care services experienced by Māori and Pacific People. In addition, we need more evidence describing the number of people with vision impairment in the general population, and access to services for all major eye conditions.
Citation: Rogers JT, Black J, Harwood M, et al. Vision impairment and differential access to eye health services in Aotearoa New Zealand: a scoping review. BMJ Public Health. 2024;2:e000313. doi: 10.1136/BMJPH-2023-000313.
Funding: This work was not funded by a specific grant from the public, commercial, or not-for-profit sectors.

by Lucy Goodman | 13 Dec, 2023 | Eye care services, Resources
 Key messages
Key messages
Limited evidence exists to describe access to eye care in New Zealand. This research has identified two major barriers that make eye health services inaccessible for some people in Aotearoa: the cost, and the lack of nearby services or transport options to reach these services
Read the published paper and download a plain language summary of the findings.
Inequities in eye health
Throughout the world, services systematically underserve some groups of people which leads to worse eye health. In Aotearoa New Zealand, the Ministry of Health has committed to addressing health inequities that are experienced by Māori, Pacific people, and people living in areas with high levels of deprivation. However, this remains a work in progress. For example, New Zealand has very little public funding for eye care services, meaning that eye care is less accessible for people who are unable to pay. Very little evidence is available describing access to eye care in New Zealand. We need this evidence so that we know how to develop services that are more accessible to everyone.
Why did we do this research?
We did this research to better understand the reasons that New Zealand’s eye care services may be difficult to use (the barriers), and ways that services may be made easier to use (the enablers), from the perspective of people who have been historically underserved.
What did we do?
We interviewed 25 people with vision problems about their opinions and experiences using eye care services. The participants all lived in an Auckland suburb that has a high level of social and economic deprivation, and most were Pacific Peoples or Māori.
What did we find?
Barriers to eye care: Most participants reported that the cost of eye care services prevented them from accessing care. Many people had to prioritise other essential costs before eye care. To overcome the cost, some had used a government loan to purchase spectacles, or purchased low-cost, premade reading glasses. Participants expressed the opinion that the government should do more to fund eye care. The distance to services and lack of transport were other commonly reported reasons participants found it difficult to reach eye care services.
Enablers to eye care: Participants were aware that good eye health is important. Some participants chose to see their GP for eye care advice. Some reported using optometry services in the past and described the experience positively. While many participants were unaware of optometry services, they were interested to understand what was involved in an eye examination. The participants also expressed how whānau (family) play an important role in their eye care.
Citation: Rogers JT, Kandel H, Harwood M, et al. Access to eye care among adults from an underserved community in Aotearoa New Zealand. Clin Exp Optom. 2023;1–9. doi: 10.1080/08164622.2023.2291527
Funding: Buchanan Charitable Foundation, The University of Auckland (Faculty Research Development Fund), Blind Low Vision New Zealand, Peter and Rae Fehl, Helen Blake QSM, Barbara Blake, and Essilor New Zealand.

by Lucy Goodman | 11 Aug, 2022 | Eye care services, Resources
In 2020, the Government of Aotearoa New Zealand proposed free annual “eye health checks” for New Zealand’s ~700,000 SuperGold card holders aged ≥65 years. To assess the evidence for this policy, we conducted a systematic scoping review of primary eye care services in Aotearoa New Zealand and ten similar high-income countries. We found that most of the countries included in the review provided subsidised eye examinations for older people. New Zealand was the only country that did not provide any eye care services for older people.
Read the published research paper and a policy brief describing the implications of this research.
Citation: Goodman L, Hamm L, Tousignant B, et al. Primary eye health services for older adults as a component of universal health coverage: a scoping review of evidence from high income countries. Lancet Reg Health West Pac. 2023;35:100560. doi: 10.1016/j.lanwpc.2022.100560
Funding: Blind Low Vision New Zealand.

by Lucy Goodman | 2 Aug, 2022 | Eye care services, Resources
Key messages:
Travel distance is unlikely to be a barrier to accessing eye health services for most New Zealanders. However, there are communities in the most deprived areas that also have long distances to travel to eye clinics. These communities are often in areas with relatively more Māori. Making eye health services more accessible for these communities should be prioritised if we are to improve eye health in New Zealand equitably.
Read the published research paper and download a plain language summary of the findings.
Why did we do this research?
Some New Zealanders face many barriers to good eye health. One of these barriers could be the distance they must travel to reach services. To make eye health services more accessible, we need to understand which communities have furthest to travel, especially when those communities may already be under resourced.
In 2022, Community Eye Health researchers published their research reporting how far New Zealanders need to travel to reach their closest eye care provider. The research showed that people living in the most deprived areas of New Zealand sometimes have the longest distances to travel to eye clinics. To achieve equity in eye care, we need to make these services more accessible.
What was the aim of this research?
The aim of this research was to find out how far people need to travel to eye clinics (optometrists and ophthalmologists) across Aotearoa New Zealand. The researchers also identified communities in the most deprived areas that were more than 50 kilometres from eye clinics, because these communities might benefit from closer services.
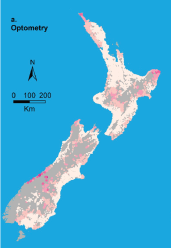
What did we do?
To understand how far people travel for eye health services, our researchers used data held by Stats NZ Tatauranga Aotearoa to count and locate all New Zealanders. They then used the addresses of all optometry and ophthalmology clinics in Aotearoa to calculate the travel distance—along our road network—between each clinic and the population. They also calculated the proportion of New Zealanders living more than 50 kilometres from clinics, and looked at distances for people living in different districts and levels of area deprivation.
What are the main results?
The researchers found 344 optometry, 46 public ophthalmology and 90 private ophthalmology clinics. Three-quarters of New Zealanders lived within 10 km of an optometry clinic and half lived within 10 km of an ophthalmology clinic. Nationally, approximately 1 in 35 people lived further than 50km from an optometry clinic compared to 1 in 14 and 1 in 10 living further than 50km from public and private ophthalmology. The researchers identified communities with high area-level deprivation that were more than 50km from eye health services. These communities were predominantly in Tairāwhiti and Northland, but there were also some in Whanganui, Hawke’s Bay, Bay of Plenty and Waikato.
Citation: Ramke J, Zhao J, Wilson O, et al. Geographic access to eye health services in Aotearoa New Zealand: which communities are being left behind? Clin Exp Optom. 2023;106:158–64. doi: 10.1080/08164622.2022.2102410
Funding: Blind Low Vision New Zealand.

 Key messages
Key messages

 Key messages
Key messages