The International Agency for the Prevention of Blindness: Challenging representation in eye health leadership
The International Agency for the Prevention of Blindness, March 2021
By Jacqueline Ramke (Associate Professor of Global Eye Health, London School of Hygiene and Tropical Medicine), Anthea Burnett (Knowledge Consultant, IAPB), Jude Stern (Head of Knowledge Management, IAPB)
A challenged world is an alert world and from challenge comes change.
When leaders reflect the populations that they serve, there can be substantial benefits. These benefits extend across health, democracy, economic growth and human development, governance, justice, and peace and security.(1) Currently, women are a minority in health leadership positions globally, which inhibits health gains among women, children and minorities worldwide.(2)
“Women belong in all places where decisions are being made” — Ruth Bader Ginsberg, 2009
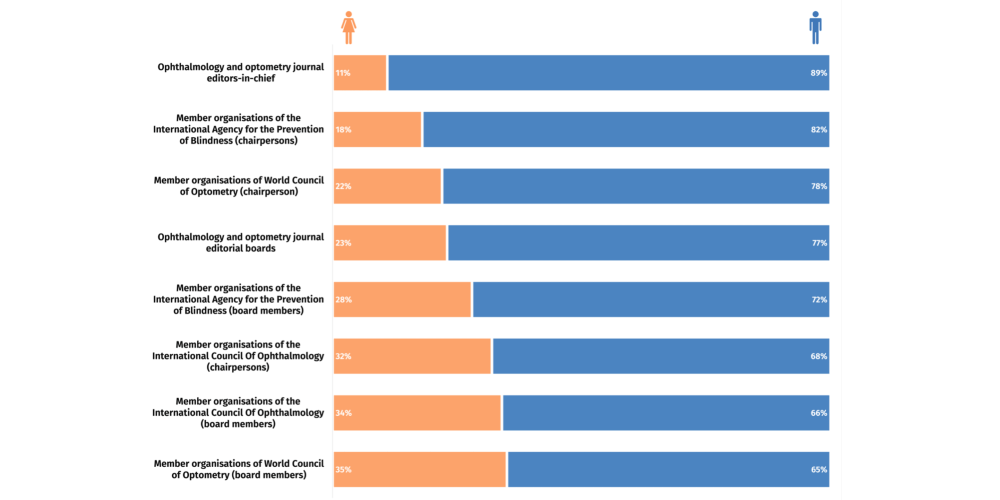
The theme of International Women’s Day this year provides the opportunity to reflect on how far we have to go in eye health to ensure enough women are in the room when decisions are being made. This is essential to address the pervasive gender inequity in eye health—in 2020, there were an estimated 112 women living with vision loss for every 100 men, even after adjusting for the longer life expectancy of women.
Read the full blog post on the IAPB website.
