Are we blinded by our measures? Refining how we assess diabetic retinopathy services worldwide

PhD candidate Nimisha Chabba presenting her work at the IAPB conference in June 2024.
PhD candidate Nimisha Chabba from the Community Eye Health team is supporting global efforts to improve eye care by refining the way that diabetic retinopathy services are monitored and reported worldwide.
Diabetes is a public health concern, as the number of people living with the disease is expected to reach 643 million by 2030. Diabetes can cause bleeding from vessels on the retina at the back of the eye (known as diabetic retinopathy), and this is the leading cause of vision loss in people of working age. Fortunately, regular eye screening and treatment can help people with diabetes to maintain good vision.
For policymakers and clinicians working to reduce vision loss from diabetes, a key priority is to gain a better understanding of access to diabetes eye care services, and how effective these services are at preserving vision. Guided by her PhD supervisors A/Prof Jacqueline Ramke and Dr Pushkar Silwal who offer their experience in eye health and health systems research, Nimisha hopes to improve the tools available to monitor diabetic eye services globally.
“We first need to understand what types of diabetic eye services are available and how many people they are reaching,” says Nimisha. “Only then can individual countries develop new and better services for people with diabetes.”
In 2022, the World Health Organization (WHO) released an Eye Care Indicator Menu (ECIM)—as the name suggests, a series of measures (known as “indicators”) that individual countries can use to monitor their own eye care services in a consistent way. Included in the Menu was an indicator to monitor retinal screening coverage—that is, the proportion of people with diabetes who have accessed these services.
Importantly, the amount of data reporting this indicator is unknown, and the first stage of Nimisha’s PhD is to address this knowledge gap by summarising all the existing literature worldwide that reports diabetic retinopathy screening coverage.
Nimisha presented the preliminary findings of her research and the plan for her PhD at the IAPB’s 2030 IN SIGHT Live meeting in Mexico City in June 2024. Of note, Nimisha described significant variability in the way that services worldwide report retinal screening coverage, which means that access to diabetic retinopathy screening cannot be easily compared between settings.
“It’s important that we have the right measures available to help countries monitor whether diabetic retinopathy services are effectively reaching the people who need them,” says eye health researcher A/Prof Jacqueline Ramke.
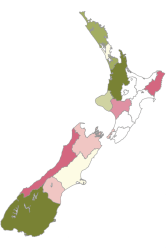
Looking towards the next phases of her PhD research, Nimisha hopes to expand WHO’s existing diabetic retinopathy indicator by developing a way to measure and assess service access concurrently with quality (known as an “effective coverage” indicator for diabetic retinopathy). To do this, she plans to collect feedback from international experts and reach a consensus about how effective coverage should be defined, and then test out the new indicator using local data from Aotearoa New Zealand. This work will have global impact by supporting the efforts of WHO and IAPB to improve monitoring and reporting of eye care services worldwide, and Nimisha is well on the way towards achieving her goals.
“Strengthening the monitoring of diabetic retinopathy services can help reduce vision loss, and I’m excited to be a part of this,” she says.
Sources:
Chabba, N. et al. What is the coverage of retina screening services for people with diabetes? Protocol for a systematic review and meta-analysis. BMJ Open 14, e081123 (2024). Read the published protocol here.